The Effects Of Crohn’s Disease On The Body
Understanding the Effects of Crohn’s Disease on the Body

Crohn’s disease is a chronic inflammatory bowel disease (IBD) primarily affecting the gastrointestinal tract. While it most commonly targets the ileum—the last part of the small intestine—it can impact any section from the mouth to the anus. This autoimmune condition causes the immune system to mistakenly attack the digestive tract, leading to inflammation, ulcers, and other complications. Although the exact cause remains unknown, genetics and environmental factors play significant roles.
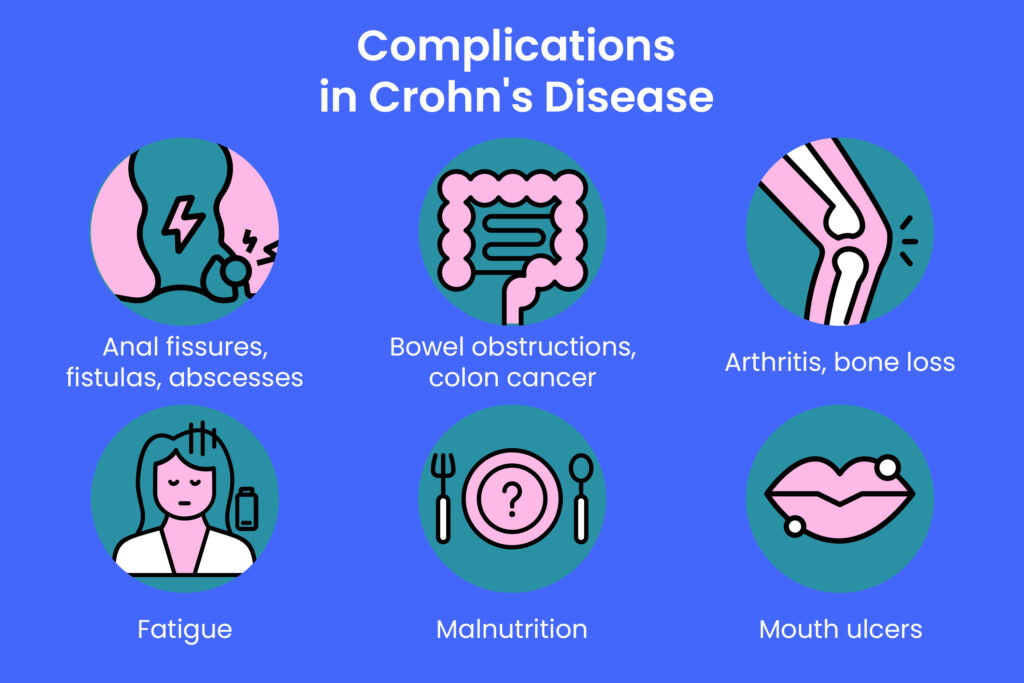
The disease is characterized by alternating periods of flare-ups and remission, with symptoms varying widely among individuals. Beyond intestinal symptoms such as diarrhea, abdominal pain, and bowel obstructions, Crohn’s disease can cause a variety of systemic effects that influence overall health and quality of life. This article explores the many ways Crohn’s disease affects the body, highlighting common symptoms, complications, and management approaches.
Fatigue: A Debilitating Symptom

One of the most frequently reported symptoms among people with Crohn’s disease is fatigue. This persistent tiredness can be both physical and mental, manifesting as low energy, poor concentration, and memory difficulties. Fatigue affects daily functioning, work productivity, and social interactions.
Research indicates that fatigue is prevalent even during remission phases, affecting nearly 40% of patients. Its causes are multifactorial, including chronic inflammation, anemia, nutrient deficiencies, psychological stress, and medication side effects. Managing fatigue often requires a comprehensive approach, including nutritional support, medication adjustments, psychological counseling, and lifestyle changes such as regular exercise, adequate hydration, and sufficient sleep.
Mouth Sores and Oral Complications

Mouth sores, or aphthous ulcers, are common in Crohn’s disease, especially among children. These painful lesions can appear on the inside of the cheeks, lips, tongue, or gums and may precede intestinal symptoms by years. Oral ulcers can impair eating, leading to nutritional deficiencies and weight loss.
Treatment typically involves topical corticosteroids or medicated mouthwashes to reduce inflammation and promote healing. Early recognition of mouth sores can assist healthcare providers in diagnosing Crohn’s disease promptly and monitoring disease activity.
Anemia and Nutritional Deficiencies

Anemia is a frequent non-intestinal complication of Crohn’s disease, often resulting from chronic blood loss, malabsorption of nutrients, or inflammation. Iron deficiency anemia is the most common type, caused by bleeding ulcers or impaired iron absorption in the inflamed gut. Vitamin B12 deficiency anemia can also occur due to damage to the ileum, where B12 is absorbed.
Symptoms of anemia include fatigue, dizziness, pale skin, and shortness of breath. Treatment involves iron supplementation, vitamin B12 injections or oral supplements, and managing underlying inflammation. Addressing anemia is crucial for improving energy levels and overall well-being.
Psychological Impact: Depression and Anxiety

Living with Crohn’s disease can take a significant emotional toll. Rates of depression and anxiety are higher among patients compared to the general population. The unpredictable nature of flare-ups, chronic pain, and lifestyle limitations contribute to psychological distress.
Stress and anxiety may exacerbate symptoms, creating a vicious cycle. Effective management includes psychological counseling, stress-reduction techniques such as mindfulness and relaxation exercises, support groups, and, when necessary, medication. Recognizing and treating mental health issues is vital for holistic care.
Bowel Obstructions and Strictures

Chronic inflammation in Crohn’s disease can cause thickening and scarring of the intestinal walls, leading to strictures—narrowed sections that obstruct the passage of food and stool. This can result in bowel obstructions, causing severe abdominal pain, bloating, vomiting, and constipation.
Strictures may be inflammatory, responding to medication, or fibrotic, requiring surgical intervention. Approximately half of Crohn’s patients develop strictures within two decades of diagnosis. Early detection and treatment are essential to prevent complications.
Diarrhea and Constipation: Opposite Challenges

Diarrhea is a hallmark symptom of Crohn’s disease, often accompanied by urgency, abdominal cramps, and weight loss. It results from inflammation, malabsorption, and increased intestinal motility. Conversely, constipation can occur due to strictures, medication side effects, or dietary changes.
Managing diarrhea involves dietary modifications such as low-fiber or low-FODMAP diets, hydration, and sometimes probiotics. Constipation management includes increasing fiber intake, fluid consumption, physical activity, and establishing regular bowel habits.
Ulcers and Fistulas

Ulcers can develop anywhere along the gastrointestinal tract in Crohn’s disease, leading to bleeding, pain, and increased risk of infection. Persistent ulcers may cause fistulas—abnormal tunnels connecting the intestine to other organs or the skin surface.
Anal fistulas are particularly common and can cause pain, discharge, and incontinence. Treatment ranges from antibiotics and immunosuppressants to surgical procedures like fistulotomy. Prompt management is necessary to prevent complications.
Vitamin D Deficiency and Bone Health

Vitamin D deficiency is prevalent in Crohn’s disease due to malabsorption, limited dietary intake, and reduced sun exposure. This deficiency contributes to bone loss, increasing the risk of osteoporosis and fractures.
Supplementation with vitamin D and calcium, along with weight-bearing exercise and minimizing steroid use, helps maintain bone health. Regular screening for bone density is recommended for Crohn’s patients.
Gallstones and Kidney Stones

Crohn’s disease increases the risk of gallstones due to disrupted bile metabolism from intestinal inflammation. Symptoms include abdominal pain, nausea, and digestive disturbances, often requiring surgical removal of the gallbladder.
Kidney stones may form due to increased oxalate absorption caused by fat malabsorption. They present with sharp flank pain, blood in urine, and nausea. Treatment depends on stone size and may involve hydration, medication, or surgery.
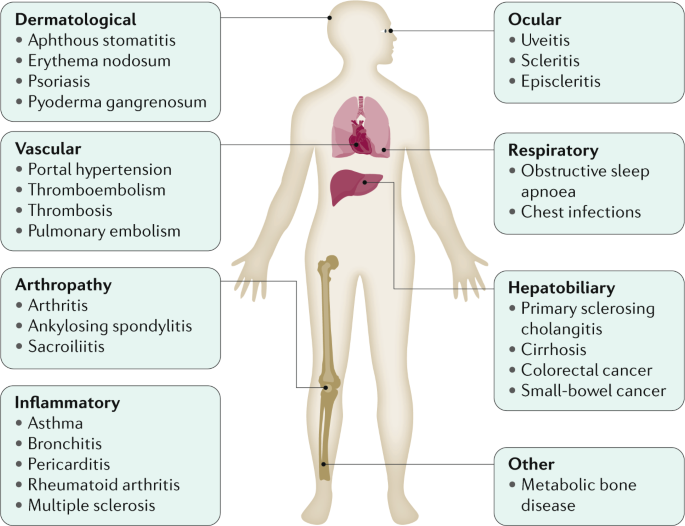
Joint Pain and Arthritis

Joint problems affect nearly half of Crohn’s patients, presenting as arthralgia (joint pain) or arthritis (joint inflammation). Large joints like knees, wrists, and ankles are commonly involved, and symptoms may fluctuate with disease activity.
Management focuses on controlling intestinal inflammation, physical therapy, pain relief, and sometimes immunosuppressive drugs. Early intervention can prevent joint damage and improve mobility.
Eye and Skin Complications

Eye inflammation, including scleritis, episcleritis, and uveitis, occurs in a subset of Crohn’s patients, causing redness, pain, and vision changes. Treatment involves controlling systemic inflammation and sometimes topical or systemic steroids.
Skin manifestations such as red bumps, blisters, and ulcers are also common. These may flare with intestinal disease or result from medications. Dermatological care and disease control are key to managing these symptoms.
Low Bone Density and Menstrual Irregularities

Low bone density affects a significant portion of Crohn’s patients, increasing fracture risk. Factors include chronic inflammation, steroid use, and nutrient deficiencies. Preventive strategies include supplementation, exercise, and lifestyle modifications.
Women with Crohn’s may experience menstrual irregularities due to hormonal imbalances, medication effects, and nutritional status. Birth control pills and careful symptom management can help regulate cycles.
Conclusion

Crohn’s disease is a complex condition that affects far more than just the digestive tract. Its systemic effects can impact energy levels, mental health, nutrient absorption, bone strength, and multiple organ systems. Understanding these diverse effects is crucial for comprehensive management and improving quality of life.
If you or a loved one is living with Crohn’s disease, staying informed about potential complications and symptoms can empower you to seek timely medical care and adopt effective lifestyle strategies. Consult your healthcare provider regularly to tailor treatments that address both intestinal and extra-intestinal manifestations of Crohn’s disease. Take charge of your health today by learning more and connecting with support networks dedicated to Crohn’s disease management.